Pakistan’s doctors are becoming some of the country’s most neglected patients, with new data presented at a national academic forum showing that nearly six out of every ten physicians are burned out, around 80 percent are physically exhausted and suicide rates among doctors are almost double those of the general population.
The warning came as senior cardiologists and mental health experts linked this crisis directly to rising heart disease, obesity, depression and anxiety among doctors, particularly in large cities like Karachi where long working hours, chronic stress, pollution, traffic and a hyper competitive medical culture have made healthy living increasingly rare.
Global health data shared at the forum showed that heart disease now kills about 21 million people each year worldwide, far more than the 3.4 million deaths recorded from Covid over three years, while stress, physical inactivity and obesity remain the main drivers of this epidemic.
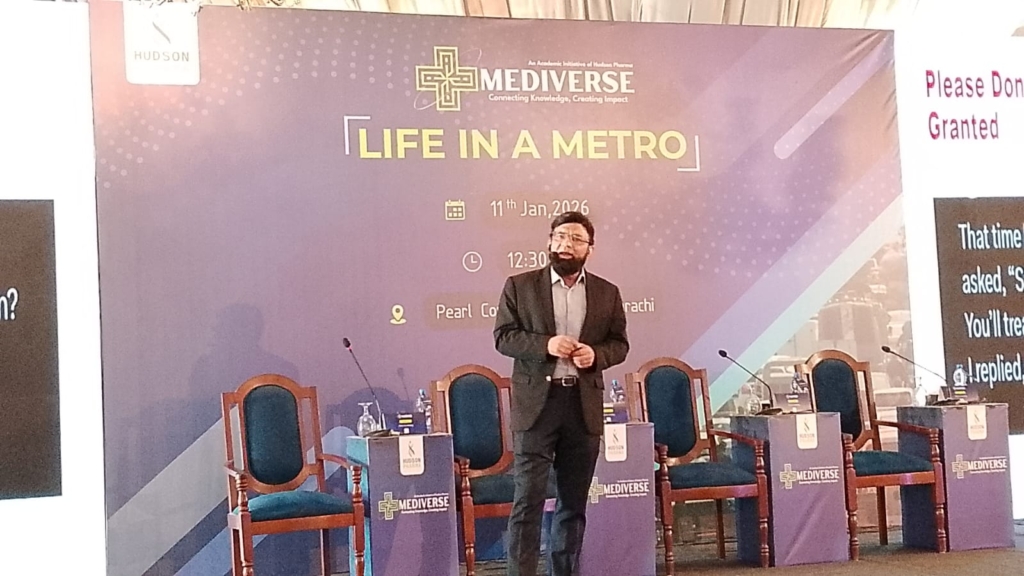
These concerns were at the centre of Mediverse Life in a Metro, a nationwide scientific symposium organised by Hudson Pharma as part of its academic initiative to promote evidence based healthcare and physician wellbeing. The Karachi session was held at Zaver Hall, Pearl Continental Hotel, and focused on how metropolitan life is accelerating both physical and emotional illness among healthcare professionals.
Delivering the keynote address, Dr Mohammad Rehan Omar Siddiqui, a consultant interventional cardiologist and internal medicine specialist, described doctors as “the most neglected patients in the healthcare system”, warning that self diagnosis, self prescribing and the culture of working through illness were pushing physicians towards early heart attacks, diabetes, depression and even suicide.

“Nearly 80 percent of doctors are already exhausted, many are overweight, and yet they continue to tell patients to exercise and lose weight,” he said, adding that chronic stress and physical inactivity directly raise the risk of hypertension, metabolic disorders and sudden cardiac events. He told the audience that most physicians no longer want their children to become doctors, not because medicine is not noble, but because the system has become punishing and unhealthy.
Dr Siddiqui said international health bodies recommend at least 180 minutes of physical activity per week, yet even among the doctors present, fewer than one in ten had exercised that day. “We are seeing brilliant neurologists and ophthalmologists dying young. We have normalised exhaustion, and that is costing lives,” he said.
Psychiatrist and psychotherapist Dr Kulsoom Haider focused on the mind body connection, explaining how emotional distress silently damages the heart and other organs. She said fear, grief and prolonged stress overwhelm the nervous system and can trigger conditions such as broken heart syndrome, while unprocessed emotions often appear as chest tightness, fatigue and gastrointestinal problems.
“The body stores what the mind cannot process,” she said, adding that depression and anxiety are now among the most common global illnesses and often show up first through physical symptoms. Simple daily practices such as controlled breathing, mindfulness, gratitude and awareness of bodily sensations, she said, help regulate the nervous system and protect both mental and cardiac health.
The panel discussion featured Dr Tanveer and Dr Afzal Lodhi, who spoke about the culture of denial within the medical profession. Dr Tanveer said he had encouraged his children to choose healthy lives rather than medical careers, stressing the need for exercise, cycling and reducing screen time. “We think nothing will happen to us. That denial is dangerous,” he said.
In her closing remarks, Samreen Hashmi Qudwai, Vice President Commercial Operations at Hudson Pharma, said doctors were more important than any brand or product, and that Mediverse was designed not just to promote scientific exchange but to remind physicians that their own health is central to the future of healthcare.
“If our doctors continue to burn out and neglect themselves, the entire system becomes unsustainable,” she warned.
Experts agreed that unless burnout, emotional exhaustion and self neglect among doctors are urgently addressed through mental health support, realistic workloads and cultural change, Pakistan risks losing its healers far too early, with serious consequences for patient safety and the country’s already fragile healthcare system.